Dietary Fiber, GI Symptoms, and Constipation
Warning
This post is not intended to diagnose or treat any medical problem. If you suspect you have a problem, consult with your primary care doctor. This post is not intended to discourage eating fiber. Instead, it clarifies some misconceptions about the benefits of adding additional fiber to our diets to alleviate constipation and its related symptoms.
I usually spend my career focusing on the first part of our GI tracts-the mouth, but today I will talk about its far end. Fiber consists of the indigestible parts of the vegetables we eat. In 1971, D.P. Burkitt proposed that a lack of dietary fiber caused diseases such as diverticulosis, hemorrhoids, and colorectal cancer, and to this day, most people agree. 1 Furthermore, it is now widely accepted that dietary fiber is a necessary component of a healthy diet and is required for normal bowel movements. 2 In other words, we increase our chances of constipation if we don't eat enough fiber. The science refutes most claims that fiber is required to be healthy. Still, it also blames fiber for many gastrointestinal symptoms like constipation, bloating, GI bleeding, and straining to move one's bowels.
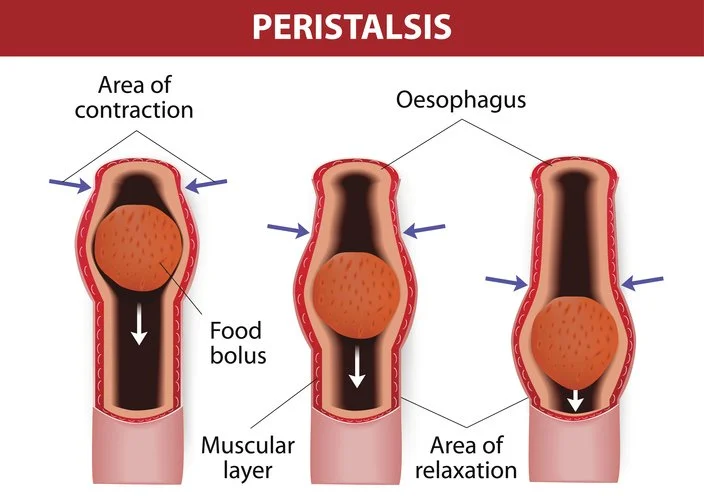
Peristalsis
The wavelike motion of our GI tracts that propel content is called peristalsis. Many believe that bulking agents like fiber aid peristalsis, but there is no proof. In fact, GI contents, including all ingested fiber, are fluid; therefore, they cannot act as solid boluses for the initiation of peristalsis. In fact, dietary fiber had been shown to retard peristalsis and hold up gaseous expulsion in humans. 3
Additionally, fiber is said to aid in water retention in the colon and results in stools that are less dry and easier to evacuate. However, the reality is that stool moisture content remains at 70%-75% regardless of the amount of fiber and water consumed 4
The Poop on Constipation
Constipation is often mistaken by the layman as the state of not passing stool, with the subsequent false notion that making more feces will allow easier excretion. In truth, constipation refers to the difficulty of evacuating a rectum packed with feces, and easier excretion cannot be affected by increasing dietary fiber, which increases bulky feces. Furthermore, it is well known that increasing dietary fiber increases fecal bulk and volume, so it is illogical to expect that bigger poops will alleviate this problem. Additionally, poops are not formed until they reach the very end of our large intestines (colons), otherwise called the rectum, or the sigmoid colon. 5 So, constipation of unknown origin (idiopathic) is truly a problem of the last part of the colon. Therefore, increasing the bulk of poops absolutely cannot help the matter. Finally, this 2006 paper concluded that low fiber intake does not equate to constipation. 6
The Singapore Fiber Study
Kok-Sun Ho and colleagues conducted research, published ten years ago, to see if eliminating fiber from the diet could alleviate constipation and its associated symptoms. They had 63 volunteers screened with a colonoscopy to rule out all known causes of constipation. Patients with colorectal cancer, previous colonic surgery, melanosis coli, or thyroid disorders were excluded. In addition, anal conditions such as severely prolapsed hemorrhoids, chronic anal fissures, or any other condition that required surgery were also excluded. So technically, the subjects all had idiopathic constipation with no known cause. Furthermore, all patients were already on a high fiber diet or taking fiber supplements.
Dietary fiber intake, symptoms of constipation, difficulty in the evacuation of stools, anal bleeding, abdominal bloating, or abdominal pain were recorded at one and six months. Then, they were asked to completely stop their dietary fiber intake for two weeks, including vegetables, cereals, fruits, whole meal bread, and brown rice. Finally, after the initial two weeks, the patients were asked to continue with as little fiber in their diet as they were comfortable with for the long term. Symptoms were recorded at one month and six months.
Results
At six months, 41 patients remained on a no fiber diet, 16 on a reduced fiber diet, and 6 resumed their high fiber diet for religious or personal reasons (Some felt uneasy not eating fiber, while others could not completely discontinue fiber due to constant media and peer pressure to increase dietary fiber).
Of those who stopped fiber completely, the bowel frequency increased from one motion in 3 and 3/4 days to one motion per day; those with reduced fiber intake had increased bowel frequency from a mean of one motion per 4 days to one motion in less than two days.
Those who remained on a high fiber diet continued to have one motion per week before and after consultation.
Bloating was absent in the no fiber group. About 31% in the reduced fiber group had bloating, while 100% in the high fiber group experienced bloating.
Finally, straining to pass stools disappeared in the no fiber group and in almost 66% of the reduced fiber group. 100% of the high fiber group experienced straining. 7
Conclusion
This study has confirmed the previously strongly held belief that the application of dietary fiber to help constipation is a myth. The study shows a strong correlation between improving constipation and its associated symptoms after stopping dietary fiber intake. Keep in mind that the study was conducted on patients with constipation. Fiber is perfectly acceptable in most healthy people's diets.
Speaking from my own two-year experiment on a zero-fiber diet (carnivore), I found I was constipated occasionally, which I had never suffered from it before. Adding back fiber seems to have made it easier for me! I have no explanation for why this happened to me. I will conclude that we are all mostly the same, but individuals all respond differently to dietary modifications. When changing something, I always assess how I respond, not how I am supposed to respond.
Finally, I left out fiber's other myth that without it, we can’t produce healthy short-chain fatty acids in the colon. You can read about it here.